- Platform
-
-
-
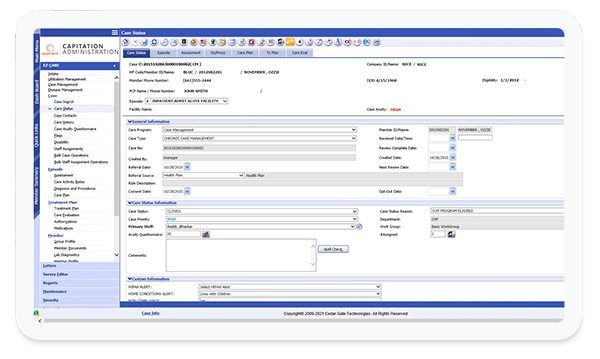
High-Performance Healthcare Platform
Discover the difference a single, integrated platform can make in your value-based care journey.
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
- Solutions
-
-
-

Markets Served
BCBS, National, Payvider, Regional
ACO, CIN, Delegated Services, FQHC, IDN, IPA, MSO, Payvider, Physician Practice
Brokers, Consultants, Employer, Payer ASO Divisions, TPAs
-
-
-

Lines of Business
Centers of Excellence, Episodes & Bundled Payment, Value-Based Benefit Design
Medi-Cal, State Medicaid
ACO REACH, CCM, MA, MCP, MSSP, PACE, PCM, TCM, TEAM & Shadow Bundles
-
-
-

Payment Models
Capitated Payments, Primary Care Attribution
-
-
-
- Company
- Resources
- Contact Us
- Client Gateway
- REQUEST A DEMO